Dementia and Alzheimer’s
Balance is defined as the ability to maintain the body’s
center of mass over its base of support.
(Shumway-Cook, 2001)
Good Balance
Exists when multiple systems interact flawlessly and automatically, providing accurate and exact information to our nervous system:
The brain receives information from our sensory receptors located in the eyes, inner ears, joints, muscles, and skin
Cognitive factors such as fear of falling, dementia, medications, and medical conditions affect balance
Receptive Communication
Requires a holistic approach:
Falls are the result of impairment in one or more complex and interrelated physiologic systems as well as environmental factors
Internal risk factors: cardiovascular, neuromuscular, orthopedic, perceptual, and psychiatric or cognitive impairments
External risk factors: medications, assistive devices, environmental hazards, and level of care
Internal Risk Factors For Falls
Internal Risk Factors |
Considerations |
|---|---|
| Cardiovascular | Dysrhythmias |
| Neuromuscular | Lower extremity weakness, loss of movement, functional decline, hypotension, CVA, Parkinson’s, stroke, neurological disorders, seizure disorder, syncope, unsteady gait, chronic/ acute conditions |
| Neuromuscular | Joint pain, arthritis, hip fracture, limb amputation, osteoporosis, foot disabilities |
| Perceptual | Impaired hearing, impaired vision, somatosensory deficits, neuropathies, dizziness/vertigo |
| Psychiatric or Cognitive | Delirium, cognitive decline, dementia, Alzheimer’s disease, depression, wandering, confusion/disorientation, fear of falling |
| Medication Side Effects | Hypotension, muscle rigidity, impaired balance, extrapyramidal symptoms (tremors, uncontrolled movements), decreased alertness |
External Risk Factors For Falls
External Risk Factors |
Considerations |
|---|---|
| Medications | Psychotropic, cardiovascular meds, diuretics, antidepressants, antianxiety/hypnotics, ETOH/drug abuse |
| Appliances and Devices | Pacemaker, cane/walker/crutch, restraints, poor-fitting wheelchair |
| Environmental Hazards | Glare, poor lighting, slippery floors, uneven surfaces, patterned carpets, foreign objects, recent move into or within a facility, proximity to aggressive patients, time of day, time since meals, type of activity, walking in a crowded area, reaching bladder/bowel urgency |
Interdisciplinary Approach.
Targeting risk factors for falls and designing intervention requires a multidisciplinary approach:
• Proper intervention has been shown to reduce falls up to 50% in high-risk groups with 3 or more falls the prior year (Ray, 1997)
• Utilization of a multidisciplinary approach to the assessment of falls means that therapy, nursing, nursing assistants, physicians, and other staff members communicate regularly.
Assessment of Risk Factors
To improve communication, designate the responsibility for assessment of the risk factors associated with falls, as shown in Table 1 and Table 2 (on the previous page) between nursing and therapy.
The Subjective Assessment
• Past medical history: diseases or disorders that lead to weakness or loss of feeling such as peripheral neuropathy, vascular disorders, and visual deficits
• Recent history of falls: where and when the falls have occurred, type of lighting, type of surface, time of day, footwear, tasks being performed
• Pain complaints or swelling complaints that can lead to decreased sensory input
Comprehensive Balance Assessment:
An Integral Part of the Physical Therapy Evaluation Subjective
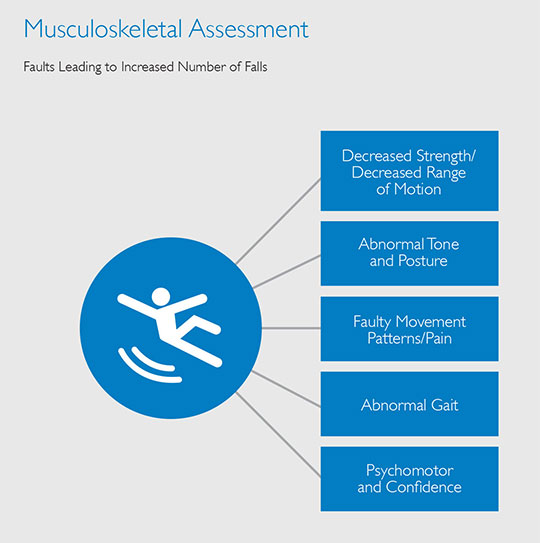
• Musculoskeletal evaluation
• Sensory systems used for balance
• Functional mobility
Review of Medications
• Particular attention to medications that affect blood pressure, cardiac function, cognition, as well as those with the side effects of dizziness and lightheadedness
• Checking vitals: temperature, blood pressure, heart rate, and respiratory rate
Strength and Range of Motion Assessment:
STRENGTH
• Manual muscle testing should be used to identify gross muscle weakness
• Focus on timing and sequence of muscle firing
• Use a closed chain or weight-bearing positions to give a better picture of functional limitations
RANGE OF MOTION
• Decreased range of motion can lead to postural compensations that affect the ability to react quickly to losses of balance
• Check Achilles tendon shortening which leads to decreased dorsiflexion, hip flexor shortening and decreasing hip extension
Muscle Tone
Abnormal tone can lead to:
• Shifting of weight away from or onto the affected side
• Loss of timing or incorrect timing of muscle contractions
• Loss of the ability to react quickly to disruptions of balance
Posture
• Postural abnormalities such as kyphosis and scoliosis
• Loss of motion in the postural muscles such as the low back, hips, legs, and ankles
Patterns And Strategies
Movement Patterns for Balance
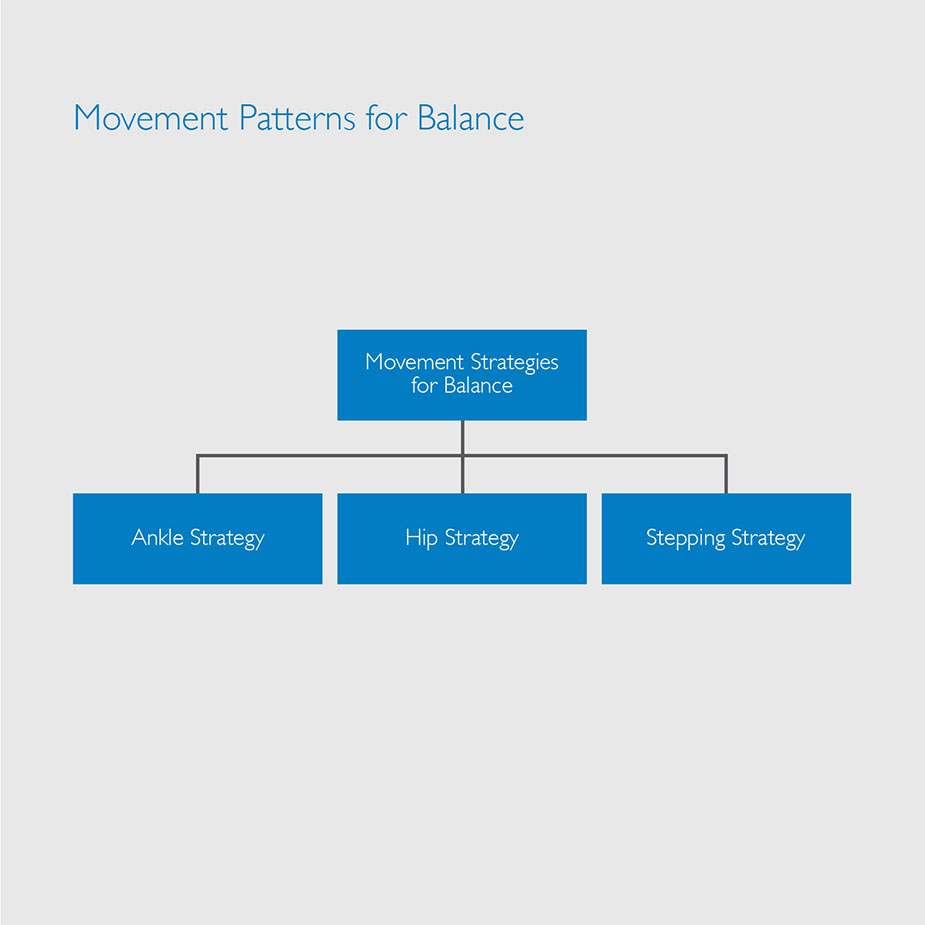
Ankle Strategy or Ankle Sway
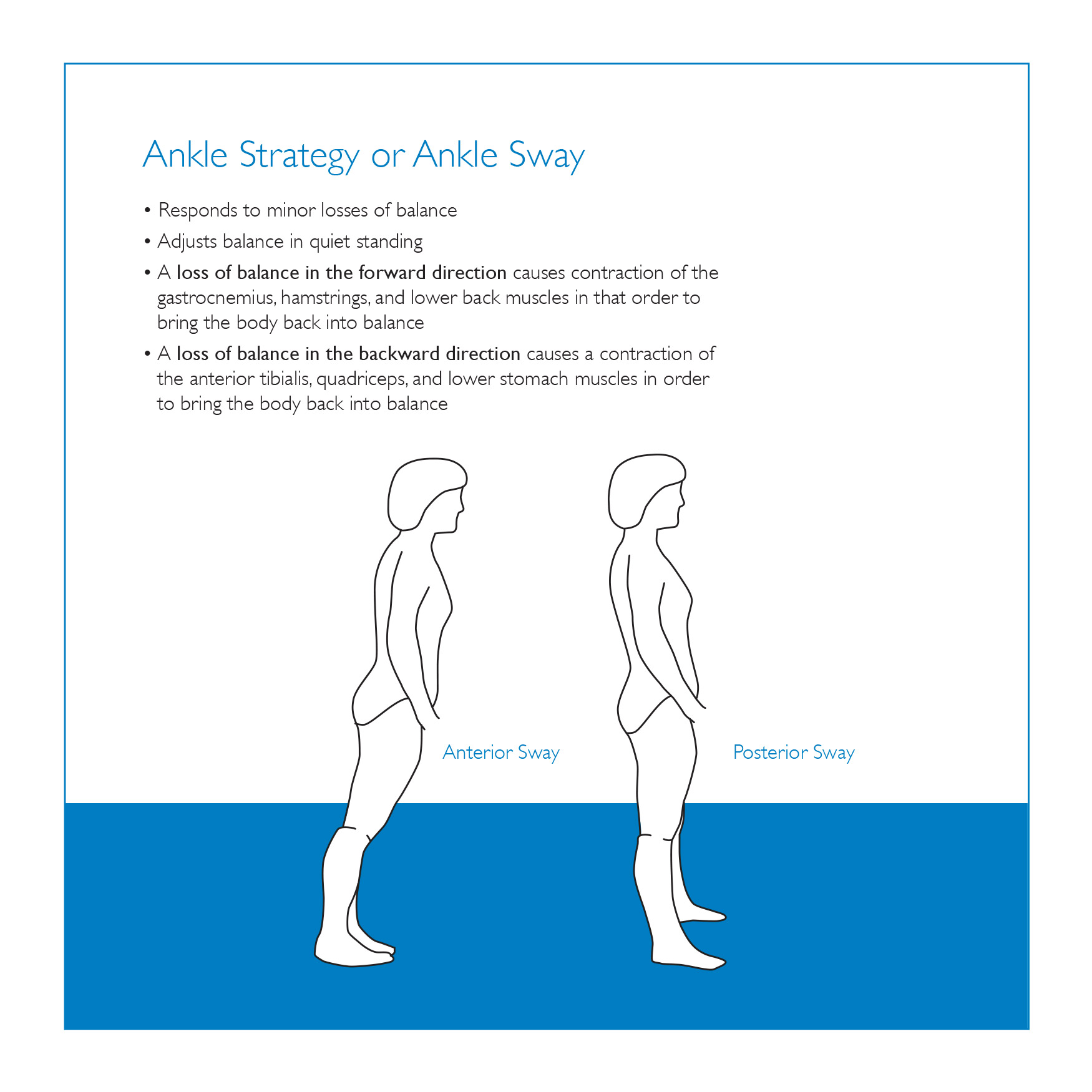
Strategies
Hip Strategy
- Used with larger losses of balance
- Activation of the muscles is from proximal to distal
- When a walker is used the body abandons the ankle strategy and relies heavily on the hip strategy
- This dependence may lead to a further loss of balance secondary to decreased ankle sway and increased ankle weakness and loss of motion
Stepping Strategy
- This strategy is used by the nervous system when the loss of balance exceeds the area of stability and the person is forced to step or fall
Pain
- Disrupts the normal function of involved joints and causes a shifting of body weight to the unaffected side
- Interrupt normal sensory and proprioceptive feedback
- Affects the ability to react appropriately to perturbations
Abnormal gait
- Decreased dorsiflexion at heel strike, decreased plantar flexion at push-off
- Decreased step length
- Decreased weight shifting
- Decreased walking speed
Walking Speed
- Reliable (Richards 1996)
- Valid (Steffen 2002)
- Sensitive (Van Lersel 1995)
- Specific (Harada 1995)
- Correlates with
• Functional ability (Perry 1995)
• Balance confidence (Mangione 2007)
Walking Speed: Predictive
• Functional and physiological changes (Perry 1995)
• Potential for rehabilitation
• Aids in the prediction of
• Falls
• Fear of falling
Confidence
Psychomotor changes include loss of confidence or changes in the client’s
perceived limits of stability
A person’s stability may be affected by fear of falling even when the physical ability exists to safely perform a task.
OR
A person may not have an accurate idea of the limits of their stability and have little sense of when loss of stability is occurring leading to falls

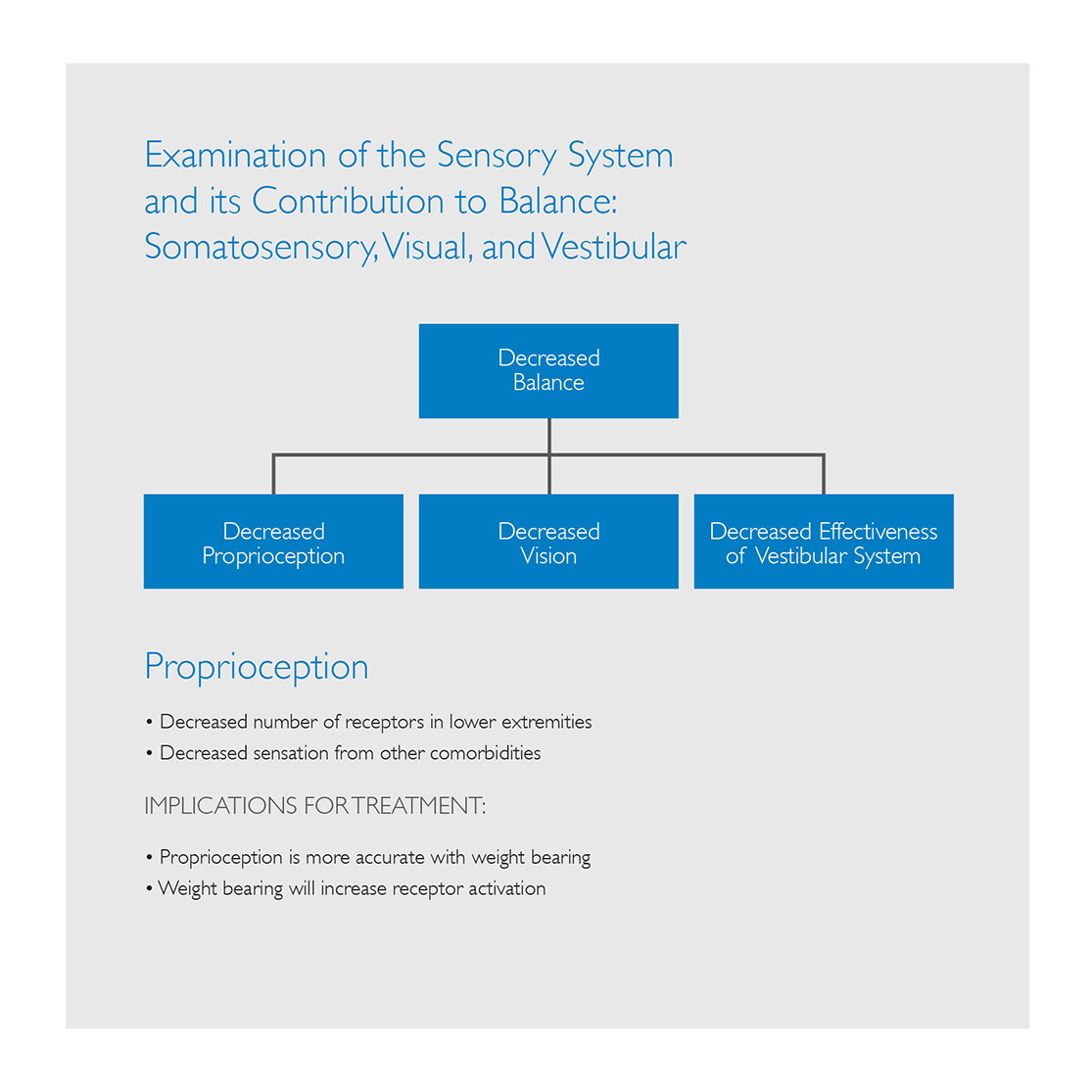
Vision
Vision declines progressively after age 50
Decreased acuity
Decreased contrast sensitivity
Decreased depth perception
Decreased glare sensitivity
Increased time required for light and dark adaptation
Decreased light entering the eye due to opacities
Aging and Vision
Impaired depth perception is one of the most common visual risk factors for multiple falls in community-dwelling older adults
What is the Vestibular System?
• 3 major components
• Peripheral sensory apparatus
• Central processor
• Mechanism for motor output
How Does Aging Affect the Vestibular System?
• Hair cells (sensory receptors) decreased by 40%
• Otolith organs
• Semicircular canals
• Permanent loss
• Neurons decrease by 3% each decade in the vestibular system
• Inactivity leads to lack of stimulus to the vestibular system
Functional Mobility Assessment
• Berg functional mobility test
• Tinetti balance tests
• Reach test
• Functional gait test/walking speed
Intervention
• Individualized treatment program
• Therapeutic exercises: strength, range of motion, coordination, static and dynamic balance, posture/alignment, as well as neuromuscular re-education
• Modifications to home environment
• Increase safety awareness
• Medication review
• Functional mobility
Treating Balance Impairments
• Rule #1: If you don’t challenge the patient they will not get better
• Rule #2: If the brain does not know what is wrong, then it wont know what to fix
• Bring the patient to their limits
• They NEED to experience a loss of balance (within a safe environment) It is those “error” messages that will “re-train” the system
• Prepare them for the “real world”
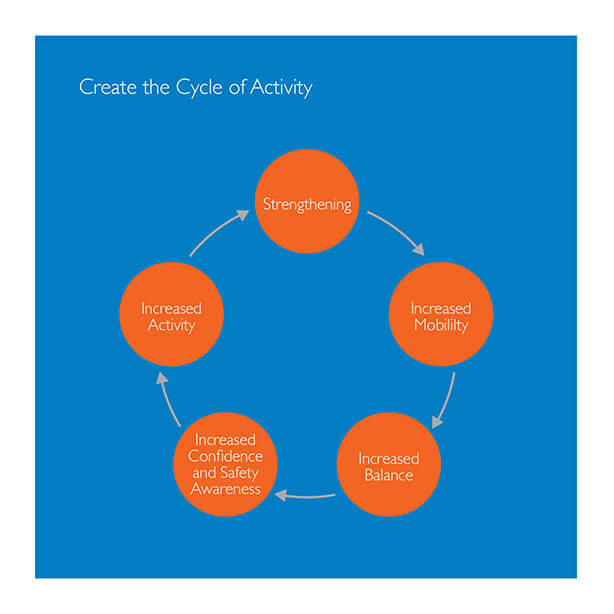
The goal Break the
Cycle Falling
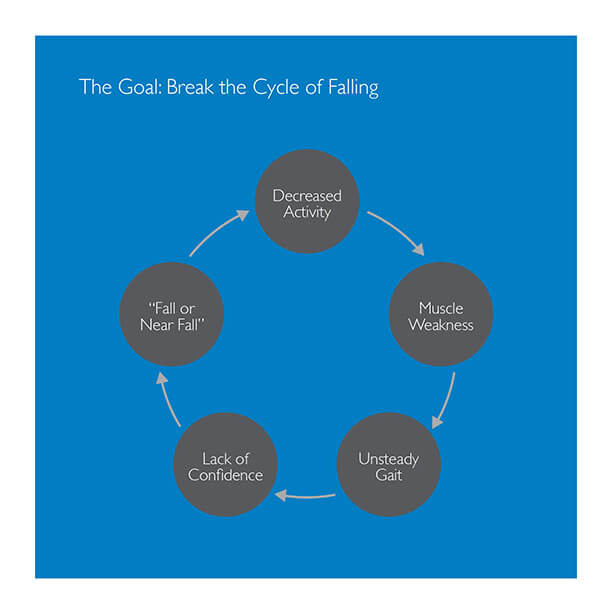
Create the cycle
Of Activity